
Lindsey and Eddie Rymer were thrilled to find out in October 2013 that they were expecting their second child. After a relatively easy pregnancy with their eldest daughter, Lucy, the Rymers had no reason to suspect things would be any different the second time around. But after their routine 20-week ultrasound with baby No. 2, Lindsey and Eddie learned that this pregnancy would be anything but smooth sailing.
Meet the Rymer family from The Mother Baby Center on Vimeo.
During the ultrasound, the obstetrician noticed something was wrong – the baby’s heart looked like it was being pushed to the side. The Rymers were referred to the Midwest Fetal Care Center in Minneapolis for a level-two ultrasound, where their baby boy was diagnosed with a congenital diaphragmatic hernia.
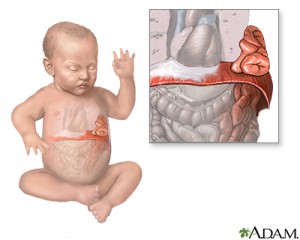 A congenital diaphragmatic hernia (CDH) is a hole in the diaphragm muscle that allows the baby’s intestines and other abdominal organs to creep up through the hole into the chest cavity. This can interfere with the growth and development of the baby’s lungs, which can lead to difficulty breathing and other serious complications. One in every 4,000 babies is born with a congenital diaphragmatic hernia. The Midwest Fetal Care Center, the only advanced fetal care center in the Upper Midwest, sees about 15-20 CDH cases each year.
A congenital diaphragmatic hernia (CDH) is a hole in the diaphragm muscle that allows the baby’s intestines and other abdominal organs to creep up through the hole into the chest cavity. This can interfere with the growth and development of the baby’s lungs, which can lead to difficulty breathing and other serious complications. One in every 4,000 babies is born with a congenital diaphragmatic hernia. The Midwest Fetal Care Center, the only advanced fetal care center in the Upper Midwest, sees about 15-20 CDH cases each year.
VIDEO: Learn more about congenital diaphragmatic hernia
“We were shocked and scared by the diagnosis,” Lindsey said. “Initially, our baby’s prognosis was not good. He had a very small lung-to-head ratio (LHR), and we didn’t know at that point if he would even make it. It was difficult to digest. But we knew that we had to give him the best chance we could and we kept fighting for him. We also knew he would need to be a fighter; that’s why we decided to name him Rocco, so he could be a rock.”

Lindsey and Eddie drew strength from their faith, family and friends as they faced the unknown ahead of them. Lindsey wore a lighthouse charm on her bracelet as a symbol of hope for Rocco. The family continued their visits to the Midwest Fetal Care Center to monitor Rocco’s progress, and after a few growth ultrasounds, doctors saw Rocco’s LHR measurements beginning to improve. Lindsey was able to carry Rocco to full-term.
“As we approached Rocco’s birth, I knew I had done everything I could at that point,” Lindsey said. “I believed in Rocco and in his care team – the rest was up to them to show us what they could do.”
On June 24, 2014, Rocco Edward Rymer was born at The Mother Baby Center, weighing a healthy 11 pounds, 3 ounces, and measuring 24 inches long.
Later that day, doctors made the decision to put Rocco on extracorporeal membrane oxygenation (ECMO), an intensive care technique designed to relieve stress on the lungs and help control blood pressure. Rocco’s surgical team would make an incision in his neck and insert tubes to circulate his blood through an artificial lung outside the body.
“ECMO is basically a heart-lung bypass machine that does the work of the baby’s heart and lungs until they can stabilize,” said Dr. Brad Feltis, surgical director of the Midwest Fetal Care Center, one of the busiest and most-experienced centers in the country dealing with congenital diaphragmatic hernias. “For CDH babies who need ECMO, the Midwest Fetal Care Center has some of the best outcomes in the country, with survival rates near 80 percent compared to the national average of 47 percent.”
“Though we hoped Rocco wouldn’t need ECMO, we knew it was the best decision for him,” Lindsey said. “Following that first 24 hours, Rocco had a pretty mellow first few days of life. We got to swab his mouth and lips with a little breast milk, take his temperature, read books to him and help the nurses with some of his care. It was encouraging to see him open his eyes and start to move his arms and legs more.”
After spending his first nine days of life on ECMO, Rocco had his surgery to repair his CDH on July 3. During the surgery, doctors found that Rocco had almost no diaphragm. They were able to put his intestines, liver, spleen and stomach back in their rightful places and used a large Gore-Tex patch to sew the diaphragm together.

Rocco’s surgery was a success, but 24 hours after the procedure, a clotting issue forced him to be emergently taken off ECMO. His team was optimistic he’d be able to remain off the heart-lung bypass machine, but Rocco was struggling with pulmonary hypertension – high blood pressure in the arteries of the lungs – and wasn’t quite strong enough on his own. He was cautiously put back on ECMO, an uncommon and risky procedure for infants, as doctors have to re-tap into the same vein in the baby’s neck.
But Rocco persevered. On July 29, he was taken off ECMO permanently. He remained in the neonatal intensive care unit (NICU) at Children’s Hospitals and Clinics of Minnesota for a few more weeks as doctors weaned him off his support and medicines. On Aug. 28, he began breathing on his own. Three days after that, Rocco “graduated” from the NICU and was transferred to the infant care center (ICC).
“It was exciting to see him meet those milestones,” Eddie said. “Once he was off ECMO, we were finally able to hold him and he was more awake and alert. We were able to change his diapers and help with occupational therapy exercises, and Lucy was able to come visit him for some playtime.”

After 88 days in the hospital, Rocco was finally discharged Sept. 20.
“It was bittersweet,” Lindsey said. “It was amazing how a place like the NICU, where no one would want their baby to end up, felt like home to us after so long.”
After 12 days at home, Rocco returned to Children’s for another surgery to insert a G-tube, or a feeding tube, inserted to help with his feedings. His surgical team also removed a lung sequestration – an abnormal formation of lung tissue – and was able to close Rocco’s abdominal muscle earlier than expected.
Today, Rocco’s prognosis is looking great. He is growing every day and has been meeting many developmental milestones that a typical 5-month-old would. He continues his occupational therapy at home to work on muscle development and strength, and while he still uses his feeding tube at night, Rocco also drinks from a bottle and should be able to move up to solids soon. Rocco will need his Gore-Tex patch checked by X-ray every six months to make sure it stays in place, but as of now his care team is optimistic that he won’t need any additional surgeries.

“It’s unbelievable to see how much progress Rocco has made, especially given his original prognosis,” Eddie said. “He’s very interactive – smiling and laughing, and sleeping almost through the night. We hope that by this time next year, he and Lucy will be able to run around and play outside together. His left lung still needs to grow a little more, and while he might not ever be a cross-country runner, I’m looking forward to bringing him out to the golf course with me once he’s old enough.”
Lindsey continues to wear the lighthouse charm around her wrist as a sign of hope, and in Rocco’s nursery hangs a picture of an anchor that says, “I refuse to sink!” The Rymers are dedicated to helping other families in similar situations and hope their story can be an inspiration for others going through similar challenges.
“I believe that Rocco’s diagnosis happened to us for a reason,” Lindsey said. “I think this was put on my plate so I could give hope to others and so that Rocco could show the world what these miracle babies can do. Each one of them deserves a chance, and we are so thankful to the Midwest Fetal Care Center and Children’s Hospitals and Clinics of Minnesota for never giving up on Rocco and for seeing us through this incredible journey.”
To see more about Rocco’s story, view our three-part video series:
- Part 1: Meet the Rymer family
- Part 2: Baby Rocco is born
- Part 3: Rocco’s ECMO procedures, surgery and recovery
The Midwest Fetal Care Center, the only center of its kind in the upper Midwest, offers prenatal diagnosis and consultation with experienced specialists and treatment for a variety of conditions.